Breath tests for lung infections
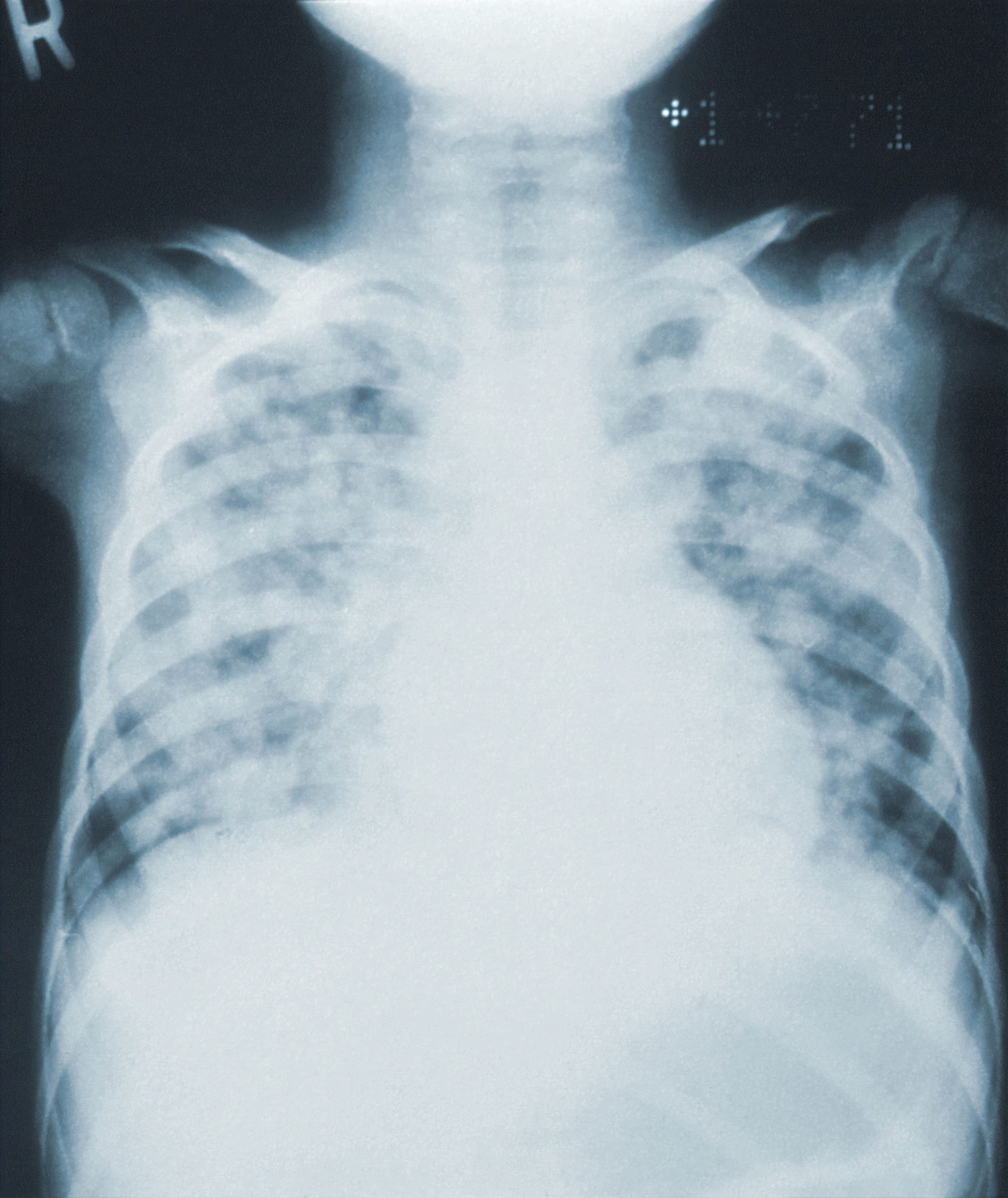
Diagnosing the cause of a lower respiratory infection is a huge challenge because all of the standard tests require successfully obtaining viable pathogens or their cellular products (like DNA or proteins) from deep in the lungs. Approximately 80% of the time clinicians have to decide on a pneumonia treatment plan before they have data on what is actually causing the infection. This leads to the over prescription of antibiotics, delays to treatments of fungal infections, lost productivity, and increased morbidity and mortality.
We are working to develop breath tests for lung infections to address the limitations of the standard diagnostics for pneumonia. Breath tests gather chemical information from the entire ventilated lungs, reflecting the biology of the pathogens and the hosts directly from the source of infection. Breath is also easily collected and an inexhaustible resource that can be sampled even from extremely ill, ventilated patients. Combined, these features of breath tests mean that we won't fail to diagnose patients because we can't access material from their infections.
Presentations
What's the Potential for Rapid, Breath-Based Diagnosis of Viral Respiratory Infections and Other Diseases?
Heather Bean, Eric Gross, and George Hanna
GERSTEL Webinars, October 2020
Podcasts
Breathtaking Biology - a metabolome adventure
Heather Bean
Ask a Biologist, May 2023
Using multi-dimensional gas chromatography to help people breathe easier
Heather Bean
Analytically Speaking, Jan 2024
Other Web Content
Breath Collection Procedure
Jenna Diefenderfer and Heather Bean
A video overview of how we collect breath samples from participants in research studies on lung infections
Breath biomarkers for early detection of CF lung infections
A primary cause of death for most persons with cystic fibrosis (CF) is respiratory failure resulting from damage caused by chronic lung infections and inflammation. More than 75% of CF patients will develop chronic Pseudomonas aeruginosa (Pa) lung infections, and Pa infection is highly correlated with worse patient outcomes. The CF Foundation recommends surveillance for lung infections at least quarterly, and to initiate antibiotic eradication therapy whenever Pa is newly cultured from CF lung specimens, whether or not the patient has symptoms of an infection. One foundational piece of the aggressive use of antibiotics for lung infections is effective, timely detection of new Pa infections, but the standard-of-care diagnostic in children (throat swab cultures) lacks sensitivity, and therefore new Pa infections can go undiagnosed for months. One of our goals is to develop breath-based diagnostics for lung infections, which don’t require the retrieval of living bacteria from the lower respiratory tract, which is the primary limitation of existing diagnostics. Therefore, breath tests could be more sensitive to new infections, shortening the time-to-diagnosis by weeks or months.
Bean began the proof-of-concept work on breath tests for lung infections when she was a Carol Basbaum Memorial CF Foundation Postdoctoral Fellow, publishing several lines of evidence from in vitro bacterial analyses and mouse lung infection models. With those studies we demonstrated that microbial and breath volatile metabolites can be used to sensitively detect and accurately identify lung pathogens. While Bean was a Postdoc at Dartmouth College, she and Dr. Jane Hill and leveraged their in vitro and mouse model data to initiate a clinical study at a CF clinic in New Hampshire, with the goal of identifying putative breath biomarkers of Pa lung infections. After Bean joined the faculty at ASU, she continued this study in collaboration with Dr. Hill (now at U. British Columbia) and Dr. Edith Zemanick (U. Colorado Denver), which has now expanded to a five-site clinical study to validate putative breath biomarkers for diagnosing P. aeruginosa lung infections, titled “IMproving P. Aeruginosa deteCTion using Breath (IMPACT-Breath; NCT04735952)”. This study has been funded by the Cystic Fibrosis Foundation (Pilot and Feasibility Award, 2016 - 2018; NIH-Unfunded Pilot Grant, 2018 - 2020; CFF Therapeutics Award 2018 – 2022), and the NIH National Heart Lung and Blood Institute (NHLBI) (R56, 2018 – 2021). Our preliminary data from 160+ breath samples show that breath biomarkers are > 95% accurate for detecting Pa lung infections.
Publications
Andrea Hahn, Katrine L. Whiteson, Trenton J. Davis, Joann Phan, Iman Sami, Anastassios C. Koumbourlis, Robert J. Freishtat, Keith A. Crandall, Heather D. Bean. (2020) Longitudinal associations of the cystic fibrosis airway microbiome and volatile metabolites: A case study. Frontiers in Cellular and Infection Microbiology. 10, 174. Link
Mavra Nasir, Heather D. Bean, Christiaan A. Rees, Edith Zemanick, Jane E. Hill. (2018) Volatile molecules from bronchoalveolar lavage fluid can “rule-in” Pseudomonas aeruginosa and “rule-out” Staphylococcus aureus infection in cystic fibrosis patients. Scientific Reports. 8, 826. Link
Heather D. Bean*, Jaime Jiménez-Díaz*, Jiangjiang Zhu, Jane E. Hill. (2015) Breathprints of model murine bacterial lung infections are linked with immune response. European Respiratory Journal. 45, 181-190. [*co-first authors] Link Editorial Feature Article: European Respiratory Journal. 45, 21-24. Link
Jiangjiang Zhu, Jaime Jiménez-Díaz, Heather D. Bean, Nirav A. Dapthary, Minara I. Aliyeva, Lennart K. A. Lundblad, Jane E. Hill. (2013) Robust detection of P. aeruginosa and S. aureus acute lung infections by secondary electrospray ionization-mass spectrometry (SESI-MS) breathprinting: From initial infection to clearance. Journal of Breath Research. 7, 037106. Link
Jiangjiang Zhu, Heather D. Bean, Jaime Jiménez-Díaz, Jane E. Hill. (2013) Secondary electrospray ionization-mass spectrometry (SESI-MS) breathprinting of multiple bacterial pathogens, a mouse model study. Journal of Applied Physiology. 114, 1544-1549. Link
Jiangjiang Zhu, Heather D. Bean, Matthew J. Wargo, Laurie W. Leclair, Jane E. Hill. (2013) Detecting bacterial lung infections: In vivo evaluation of in vitro fingerprints. Journal of Breath Research. 7, 016003. Publisher Featured Article Link
News
ASU researcher starts clinical study to improve diagnostic tests for lung infections
Our work got a shout-out at the 2023 North American Cystic Fibrosis Conference plenary:
"Micro-management": The changing face of infections in CF
Breath biomarkers for diagnosing Valley fever
Coccidioidomycosis, or Valley fever, is a fungal pneumonia that is highly prevalent in the desert regions of North and South America, with an estimated 350,000 annual cases. In endemic and highly populated areas, e.g., Phoenix and Tucson, up to 30% of community-acquired pneumonias may be caused by Valley fever. The current diagnostics for Valley fever are severely lacking due to poor sensitivity (diagnosis via serology) and invasiveness (via biopsy); therefore, the infections are difficult to diagnose and often mistaken for a bacterial pneumonia and inappropriately treated with antibiotics. The lack of a suitable diagnostic strongly contributes to an unacceptable 23 day median time-to-diagnosis, which costs Arizonans more than $100M annually in medical costs and lost productivity. Our goal is to substantially shorten the time-to-diagnosis for Valley fever through the development of sensitive and specific breath-based diagnostics. With funding from the Arizona Biomedical Research Centre (2018 - 2022), we are leading a team of researchers from ASU, Northern Arizona University, and Mayo Clinic to characterize the volatile metabolomes of the two species that cause Valley fever, Coccidioides immitis and C. posadasii, via analysis of in vitro cultures, mouse model lung infections, and human lung specimens.
Publications
Jenna Diefenderfer, Heather D. Bean, Emily A. Higgins Keppler. (2024) New Breath Diagnostics for Fungal Disease. Current Clinical Microbiology Reports, in press. Link
Emily A. Higgins Keppler, Marley C. Caballero Van Dyke, Heather L. Mead, Douglas F. Lake, D. Mitchell Magee, Bridget M. Marker, Heather D. Bean. (2023) Volatile Metabolites in Lavage Fluid Are Correlated with Cytokine Production in a Valley Fever Murine Model. Journal of Fungi, 9, 115. Published: Link
Emily A. Higgins Keppler, Heather L. Mead, Bridget M. Barker, Heather D. Bean. (2021) Life cycle dominates the volatilome character of dimorphic fungus Coccidioides spp. mSphere. 6, e00040-21. Link
Heather L. Mead, Chandler C. Roe, Emily A. Higgins Keppler, Marley C. Caballero Van Dyke, Klaire L. Laux, Aubrey L., Funke, Karis J. Miller, Heather D. Bean, Jason W. Sahl, Bridget M. Barker. (2020) Defining critical genes during spherule remodeling and endospore development in the fungal pathogen Coccidioides posadasii. Frontiers in Genetics. 11, 483. Link
Presentations
Dusty Devil: Improving tests for Valley fever
Heather Bean & Mitch Magee
A Sip of Science, presented by The Biodesign Institute at ASU, Sep 2022
Characterizing in vitro and in vivo biomarkers for a Valley fever breath test
Emily Higgins Keppler
65th Annual Coccidioidomycosis Study Group, Apr 2021
Breath tests to diagnose VF and measure disease burden
Heather Bean
NASEM Workshop on Impact and Control of Valley Fever, Nov 2022
Identifying breath biomarkers for lung infections using two-dimensional gas chromatography
Heather Bean
Biodesign China Symposium, Jan 2022